Building a stronger health ecosystem in Malawi
In the face of budget constraints and competing health priorities, Malawi faces tough decisions in its pursuit of improving health care for its people. However, the country is investing in multiple initiatives and has developed a new financing strategy to drive much-needed change
Like many low- and middle-income countries, Malawi is undergoing an epidemiological and demographic transition. Non-communicable diseases now constitute 33.4% of the disease burden, up from 22.1% in 2010, and communicable diseases comprise 43.4% of the disease burden, down from 57.8% in 2010. In addition, maternal and neonatal conditions rank first as a single cause of the burden of disease, at 13.8%. Malawi’s total health expenditure per capita is estimated at $39.90, where it has stagnated for two decades. This is mostly owing to its rapidly growing population, which is expanding by 2.6% per annum. The population is largely youthful, with 80% of its people aged below 35 years and a median age of 17. Although the youthful population presents a huge opportunity for the country, there is also the problem of a high teenage pregnancy rate, which stands at 29%.
Investing in change
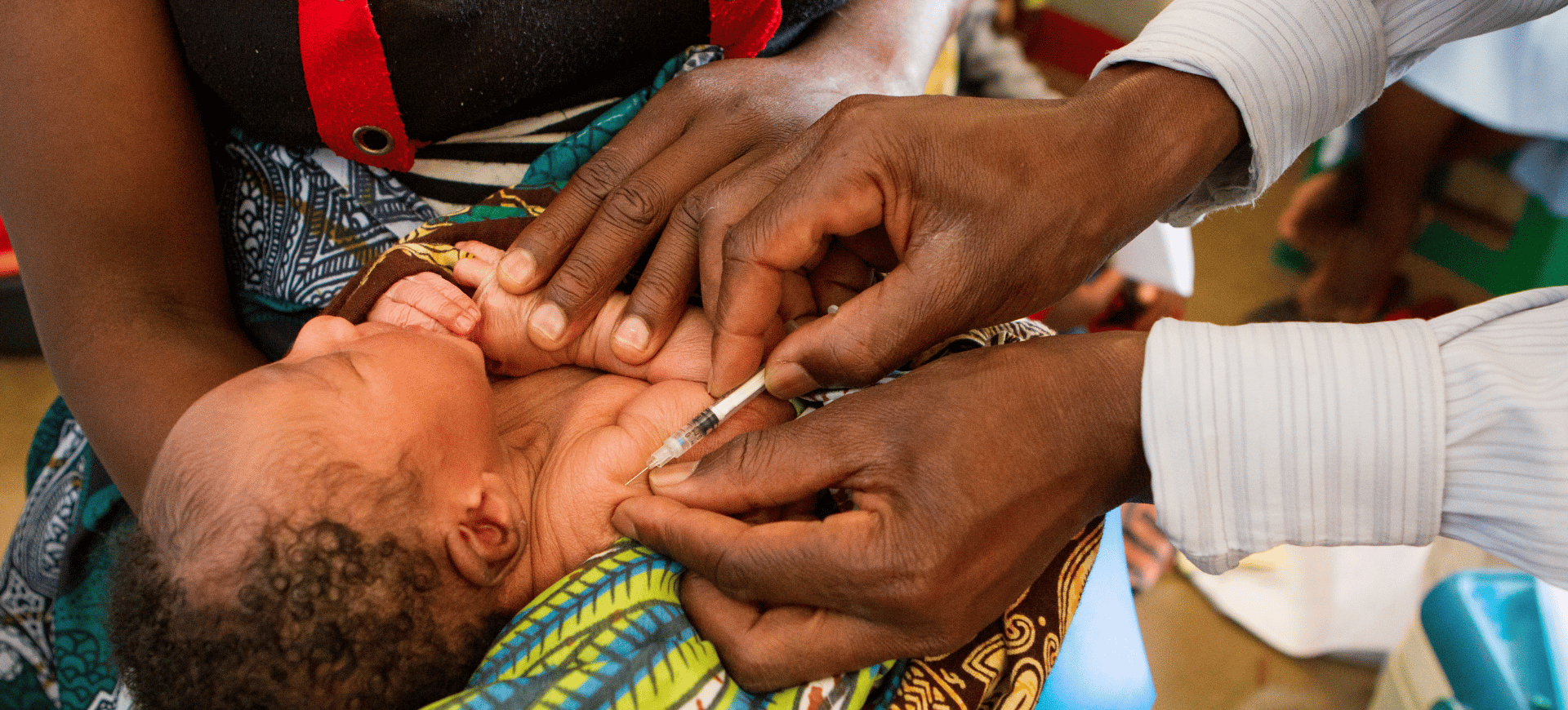
Malawi has invested in a primary healthcare system as a cost-effective platform for tackling the multipronged burden of disease. The primary healthcare system consists of nearly 500 health centres and 90 health posts, and about 15,000 health surveillance assistants who anchor the community health system and provide community promotion and preventive health services across the country. The Ministry of Health introduced the Integrated Community Health Information System to support integrated and timely reporting of community health data and to support disease surveillance. The ministry aims to construct 900 health posts in hard-to-reach areas and increase the number of health surveillance assistants to meet a 1:1,000 HSA to population ratio and increase the number of community midwife assistants and community nurses. It is also the government’s priority to provide the necessary equipment, supplies and supportive supervision for the HSAs. Malawi’s primary healthcare system also provides a platform for multisectoral action on population management, nutrition, and maternal and child health.
Given the multipronged disease burden, the Malawi Health Sector Strategic Plan III (2023–2030) has proposed the integration of health service delivery and a client-centred approach. The Ministry of Health is therefore piloting the integration of outreach clinics to communities and pathways at the health centre level. The design of the integration implementation has involved health workers and communities in order to build ownership and trust. The ministry has also commenced a holistic review of health worker cadres in order to respond to the multifaceted disease burden and to prepare a workforce at the primary level that will be capable of managing non-communicable diseases and pandemics.
Repairing and rebuilding
The Covid-19 pandemic and recurring adverse weather events have caused so much loss to Malawi. Lives have been lost, health has been diminished, livelihoods have been deprived and the provision of health has been disrupted. The government has thus embarked on efforts to strengthen pandemic preparedness through enhanced disease surveillance, implementation of a One Health system, the establishment of infectious disease treatment centres at tertiary hospitals and isolation centres in districts, and the building of a response team that is ready to deploy immediately when a pandemic or climate-related emergency arises.
Malawi faces many difficult political choices, given the prevailing health sector situation. Chief among these is what should be financed from the national budget, given the low level of health financing, broadly, and domestic financing, particularly. With an increasing population, a multifaceted disease burden, and a stagnant total health expenditure per capita, explicit choices must be made about what package of services will be delivered using the government budget and how services outside that benefit package will be paid for. The Ministry of Health has developed a national health financing strategy that has proposed many reforms to attempt to address the situation. The strategy will explore earmarked taxes for health, and strengthen equitable financing mechanisms in order to capture individuals who do not contribute according to their capacity to pay. The ministry is also engaging the private sector to strengthen public-private collaboration in delivering and financing health care. The decision on how much to invest at the primary level versus the higher levels is also a critical one.
On the one hand, the country could invest in more highly skilled health workers at the primary level to strengthen gatekeeping to the higher levels, but that may be costly. On the other hand, the country could maintain the status quo and risk poorer outcomes or congested secondary and tertiary health facilities.